Sexually Transmitted Infections
Sexually Transmitted Infections (STIs) affect all genders and are spread through sex or other intimate contact. There are at least 20 STIs, many of which require different prevention strategies. If you are sexually active, the only way to know your status is to get tested regularly (BC Centre for Disease Control, 2016). Many people get tested after having sex with every new sex partner, and for others, this is not practical and they may get tested every few months instead. See the sexual health resources page for information on sex-positive places to get tested in Toronto.
Some of the most common STIs and prevention strategies are listed below:
Chlamydia
Transmission
Chlamydia is a sexually transmitted infection (STI) caused by the bacteria Chlamydia trachomatis. Infections can occur in the penis or external genitals, vagina or internal genitals, anus, throat, and eye. The bacteria can also be found in body fluids such as semen, pre-ejaculate, vaginal fluids, and anal fluids.
You get chlamydia through vaginal, oral, and anal sexual contact. This includes both penetrative sex and sexual activities where there is an exchange of body fluids. You can also get chlamydia by sharing sex toys. If you have chlamydia, you can pass it to others even if you don’t have symptoms.
Prevention
It is a good idea to be tested regularly for STIs, especially if you have new sexual partners or open relationships. Talking with partners about safer sex makes sure everyone knows what to expect. Condoms are great if they work for you – the correct use of condoms reduces your chances of getting and passing chlamydia.
Symptoms
If you have chlamydia, it is common to not notice any symptoms. If you do get symptoms, they will most likely show up between 2 and 6 weeks after sexual contact. Your symptoms will depend on where the infection is located. The most common symptoms include:
Penis/external genitals: You may notice abnormal discharge and an unusual, painful, or itchy sensation. You could also have pain or trouble when urinating. If you have testicles you may experience pain there and sometimes a little swelling.
Vagina/internal genitals: You may notice abnormal discharge and bleeding. Other symptoms would be lower abdominal pain and sometimes pain during sex.
Anus: You may notice abnormal discharge. You can also have pain in the area.
Throat: It is rare to have symptoms here but you might experience a sore throat.
Eye: You may notice swelling or abnormal discharge.
*Note: If you have had lower surgery, your genital symptoms may vary.
Testing
Testing is usually done with a urine sample or a swab of the throat, rectum or vagina. It is best to get tested for chlamydia if you:
have symptoms
have a sexual partner who has tested positive for chlamydia
are doing routine screening for STIs
are pregnant
are going to have an IUD inserted, a surgical abortion, or a gynecological procedure
Window Period (how long to wait before testing): Most test results are accurate 2 to 6 weeks after you come in contact with chlamydia.
Pregnancy: If you are pregnant, you should be screened for chlamydia. You can pass chlamydia to your child during birth.
Treatment
Chlamydia is treated with prescription antibiotics. It is important to take your medications as directed. If you miss any doses, the infection may not be cured. See your health care provider if this happens or if you still have symptoms after you finish your treatment.
Your sexual partners within the last two months should be tested and treated for chlamydia. If you haven’t had sex in the last two months, your last partner should be tested and treated.
It is important to not have sex (even with a condom) for 7 days after the start of your treatment. If you do have sex, you could pass chlamydia to your sexual partners or get it again. If this happens, talk to your health care provider.
(BC Centre for Disease Control, 2016)
Gonorrhea
Transmission
Gonorrhea is a sexually transmitted infection (STI) caused by the bacteria Neisseria gonorrhoeae. This infection can occur in the penis or external genitals, vagina or internal genitals, anus, and eye. The bacteria can also be found in body fluids such as semen, pre-ejaculate, vaginal fluids, and anal fluids.
Gonorrhea is passed through vaginal, oral, and anal sexual contact. This includes both penetrative sex and sexual activities where there is an exchange of body fluids. You can also get gonorrhea by sharing sex toys. Once you have this infection, you can pass it to others even if you don’t have symptoms.
Prevention
It is a good idea to be tested regularly for STIs, especially if you have new sexual partners or open relationships. Talking with partners about safer sex makes sure everyone knows what to expect. Condoms are great if they work for you – the correct use of condoms reduces your chances of getting and passing gonorrhea.
Symptoms
If you have gonorrhea, it is common to not notice any symptoms. If you do get symptoms, they will most likely show up between 2 to 7 days. Your symptoms will depend on where the infection is located, but occur most often in the penis/external genitals. The most common symptoms include:
Penis/external genitals: You may notice abnormal discharge and an unusual, painful, or itchy sensation. You may also have pain or trouble when urinating. If you have testicles you may experience pain and sometimes a little swelling in the area.
Vagina/internal genitals: You may notice abnormal discharge and bleeding. Other symptoms may include lower abdominal pain and sometimes pain during sex.
Anus: You may notice abnormal discharge. You can also have generalized pain in the area.
Throat: It is rare to have symptoms, but you might experience a sore throat.
Eye: You may notice swelling or abnormal discharge.
*Note: If you have had lower surgery, your genital symptoms may vary.
If you treat gonorrhea early, there are usually no other health problems. If left untreated, it can lead to serious complications including:
higher chance of getting and passing HIV
infertility
ectopic pregnancy
chronic pelvic pain
reactive arthritis
Testing
There are choices for how you test for gonorrhea. A health care provider will recommend certain tests depending on the types of sex that you’re having. Testing is usually done with a urine sample or a swab of the throat, rectum or vagina.
It is best to get tested for gonorrhea if you:
have symptoms
have a sexual partner who has tested positive for gonorrhea
are doing routine screening for STIs
are pregnant
are going to have an IUD inserted, a surgical abortion, or a gynecological procedure
Window Period (how long to wait before testing): Most test results are accurate 7 days after you come in contact with gonorrhea.
Treatment
Gonorrhea is treated with prescription antibiotics. It is important to take all your medications as directed. If you miss any doses, the infection may not be cured. See your health care provider if this happens or if you still have symptoms after you finish your treatment.
It is important to not have sex (even with a condom) for 7 days after the start of your treatment. If you do have sex during this time, you could pass gonorrhea to your sexual partners or get it again. If this happens, talk to your health care provider.
If you test positive, your sexual partners within the last two months should be tested and treated for gonorrhea. If you haven’t had sex in the last two months your last partner should be tested and treated.
(BC Centre for Disease Control, 2016)
Herpes
Transmission
Herpes is a sexually transmitted infection (STI) caused by the virus Herpes Simplex Virus (HSV). It can occur on the skin around or sometimes inside the penis or external genitals, vagina or internal genitals, anus, and mouth. For many people, herpes is a skin condition that comes and goes without causing problems. Herpes is a very common STI. While it cannot be cured, it can be managed.
HSV-1 is commonly found around the mouth and is often called "cold sores". It can be passed orally by kissing and it can be passed to the genitals through oral sex. HSV-2 is commonly found in the genital area and is passed through vaginal and anal sex, but it can also be passed to the mouth through oral sex. It is uncommon for HSV-2 to be found on the lips, but it is becoming more common to find HSV-1 in the genital area. Both types are sometimes passed to other areas of the body through skin-to-skin contact.
After the first outbreak, herpes stays in the body and becomes inactive. The virus may become active from time-to-time. When this happens, symptoms usually show up in the same general area as the first time. There is no way of knowing if, or how often, a person will have future outbreaks. For most people, outbreaks happen less often over time.
Herpes is passed through vaginal, oral, and anal sexual contact. This includes both penetrative sex and sexual activities where there is skin-to-skin contact. The contact needs to be directly with the part of the body where a person has the virus.
Herpes can be passed to others even if you don’t have symptoms. The virus can be found on the skin even when there are no symptoms, called "asymptomatic shedding". However, it’s more likely to be passed when symptoms are present.
Once you have one type of HSV, it is unusual to get the same type on another area of your body. The exception is within the first few months after you are exposed to HSV, while your body is building up antibodies to the virus. HSV can be passed to other parts of the body during this time. Try not to touch the sores and wash your hands often, to lower the chances of passing it to another part of your body.
If you have one type of herpes, then it is not possible to get that same type again.
Prevention
To lower the chances of passing or getting herpes:
you can still be sexual when you have an outbreak, but take care to avoid skin-to-skin contact in the area where you have sores (for example, do not give oral sex when you have a sore on your mouth)
consider antiviral medication if you have frequent outbreaks
It is a good idea to be tested regularly for STIs, especially if you have new sexual partners or open relationships. Talking with partners about safer sex makes sure everyone knows what to expect. Condoms are great if they work for you – the correct use of condoms might reduce your chance of getting and passing herpes (depending where outbreaks are located).
Symptoms
If you have herpes, it is common to not notice any symptoms. If you do get symptoms, they will most likely show up between 2 to 21 days after sexual contact.
The first time you come in contact with the virus and get symptoms is called a primary outbreak. The first outbreak can last longer and be more severe than future outbreaks. Early symptoms include itching, burning, or tingling at the site where blisters or sores may appear, followed by painful red sores or tiny blisters and sometimes swollen glands, fever and body aches. You may have severe flu-like symptoms, such as fever, headache and muscle aches. Over time, outbreaks usually happen less often and the symptoms are milder.
Herpes outbreaks may be triggered by different things. These can include sun exposure, lack of sleep, alcohol use, skin irritation, and stressful events. Symptoms may be reduced by using sunscreen, getting enough sleep, drinking water, using lube, eating well and using coping strategies for stress.
Testing
Most testing for herpes is done by an exam and a swab taken from a blister. Results are the most accurate if you see a health care provider as soon as a sore develops. They will look at the sore to determine what it is. If possible, they will take a swab. There is a blood test for herpes but it is not routinely done. It is best to get tested for herpes if you have symptoms.
Treatment
You can choose if you want to treat herpes. Symptoms will go away without treatment, though they may go away sooner with treatment. Herpes is treated with prescription antiviral medications. These medications can lessen the severity of an outbreak and lower the chances of passing it to sexual partners. Medication works best if it is started as soon as possible after an outbreak begins.
(BC Centre for Disease Control, 2016)
HPV
Transmission
Human papillomavirus (HPV) is a sexually transmitted infection (STI) that can occur in the penis or external genitals, vagina or internal genitals, anus, and throat. There are over 40 different types of HPV that can cause infections in these areas.
Some types of HPV cause genital warts. Other types of HPV are more serious and may cause cancer of the cervix, anus, vagina/internal genitals, penis/external genitals, genital area, and throat. This page has information only about HPV strains that may cause cancer.
HPV can be managed.
HPV is passed though vaginal, oral, and anal sexual contact. This includes both penetrative sex and sexual activities where there is skin-to-skin contact. You can also get HPV by sharing sex toys. If you have HPV, you can pass it to others even if you don’t have symptoms.
Prevention
The HPV vaccine can help prevent most genital cancers and genital warts. This vaccine is available for people of all genders. The vaccine will not help get rid of an existing HPV infection, but it can prevent future infections.
It is a good idea to be tested regularly for STIs, especially if you have new sexual partners or open relationships. Talking with partners about safer sex makes sure everyone knows what to expect. Condoms are great if they work for you – the correct use of condoms may reduce your chance of getting or passing HPV.
Symptoms
If you have HPV, it is common to not have any symptoms. If you do get symptoms, the type of symptoms will depend on where the infection is located.
Testing
There is currently no routine test for HPV in Ontario. Instead, a Pap test is used to screen for cancerous changes in cells.
People with a cervix should have regular cervical Pap testing done, as recommended by BC Cancer. If you have receptive anal sex or are living with HIV, some health professionals may recommend that you have regular anal Pap testing. Talk to your health care provider to figure out what’s best for you.
Treatment
Most HPV infections go away on their own and do not need treatment. If an HPV infection persists, there are different ways that the cancerous changes in the cells can be treated, depending on how severe the changes are.
If you have an abnormal Pap result, you may need to have a Pap test more often or go for additional testing. Pap tests often find changes early enough that treatment can be given before cancer develops.
(BC Centre for Disease Control, 2016)
HIV/AIDS
Transmission
Human Immunodeficiency Virus (HIV) is a virus that targets the body’s immune system. It is passed through blood and body fluids such as semen, pre-ejaculate, vaginal fluids, anal fluids, and breast/chest milk. HIV can be managed with antiviral medications.
HIV is passed through vaginal and anal sexual contact. This includes both penetrative sex and sexual activities where there is an exchange of body fluids. There is a very low chance that HIV may be passed through oral sex or when using sex toys.
HIV can also be passed through sharing drug equipment, such as needles.
HIV does not live for long outside the body. It cannot be spread by casual contact such as kissing or sharing drinking glasses with someone who has HIV.
If you have HIV, you can pass it to others even if you don’t have symptoms.
If HIV is treated early on, you are less likely to have other health problems. Early treatment helps to keep your immune system healthy. Taking medication early will also lower the chances of passing HIV to other people.
If left untreated, HIV can lead to serious complications.
If HIV weakens your immune system, it makes it easier to get infections or cancers that rarely occur in people with healthy immune systems. Having HIV does not mean you have AIDS. AIDS occurs when your immune system has been severely weakened by HIV. Even without treatment, it takes a long time for HIV to progress to AIDS, usually 10 to 12 years.
Prevention
To help prevent getting HIV, you can:
use condoms
consider pre exposure prophylaxis (PrEP)
consider post exposure prophylaxis (PEP)
if you use drugs, do not share drug equipment such as needles or straws
use new drug equipment every time you use drugs
get tested for other STIs, because they can increase your chance of getting (or passing) HIV
It is a good idea to regularly test for STIs, especially if you have new sexual partners or open relationships. Talking with partners about safer sex makes sure everyone knows what to expect. Condoms are great if they work for you – the correct use of condoms reduces your chances of getting and passing HIV.
Symptoms
It is common to not notice any symptoms or to mistake HIV symptoms for a different illness. If you do get early symptoms, they will most likely show up between 2 to 4 weeks after sexual contact. Common early symptoms of HIV infection are called seroconversion illness. These symptoms include:
fever
sore throat
headache
muscle aches and joint pain
swollen glands
Testing
HIV testing is done with a blood sample. Tests either look for antibodies or a small amount of the virus itself. HIV antibodies are made by the immune system to fight the virus.
There are options for how to test for HIV, including:
A blood sample is taken from the arm and is sent to a laboratory for testing.
A drop of blood is taken from the finger and results are available in a few minutes. This is called the point of care (POC) test or rapid test. This test has a longer window period, meaning it takes longer before the results are accurate. POC testing is usually used as a screening test, so a blood sample will also need to be drawn.
Everyone should be tested for HIV at least once in their life. Talk to your health care provider about how often you should test. In general, it is best to get tested for HIV if you:
have symptoms
have a sexual partner who has tested positive for HIV
have shared drug equipment such as needles
are doing routine screening for STIs
are pregnant
Some clinics offer anonymous HIV testing.
Window Period (how long to wait before testing): There are different types of tests for HIV. Depending on the type of test used, most test results are accurate 3 weeks after you come in contact with HIV, but it can take up to 3 months. In British Columbia, most test results should be ready in 10 days.
Pregnancy: If you are pregnant, you should be screened for HIV. You can pass HIV to your child during birth and through breast-/chest-feeding.
Treatment
If you have been diagnosed with HIV, your sexual partners should be tested. The chance of passing HIV to partners depends upon many factors, such as the level of HIV that a person has in their body (HIV viral load), the type of exposure, and whether a condom was used.
(BC Centre for Disease Control, 2016)
Birth Control
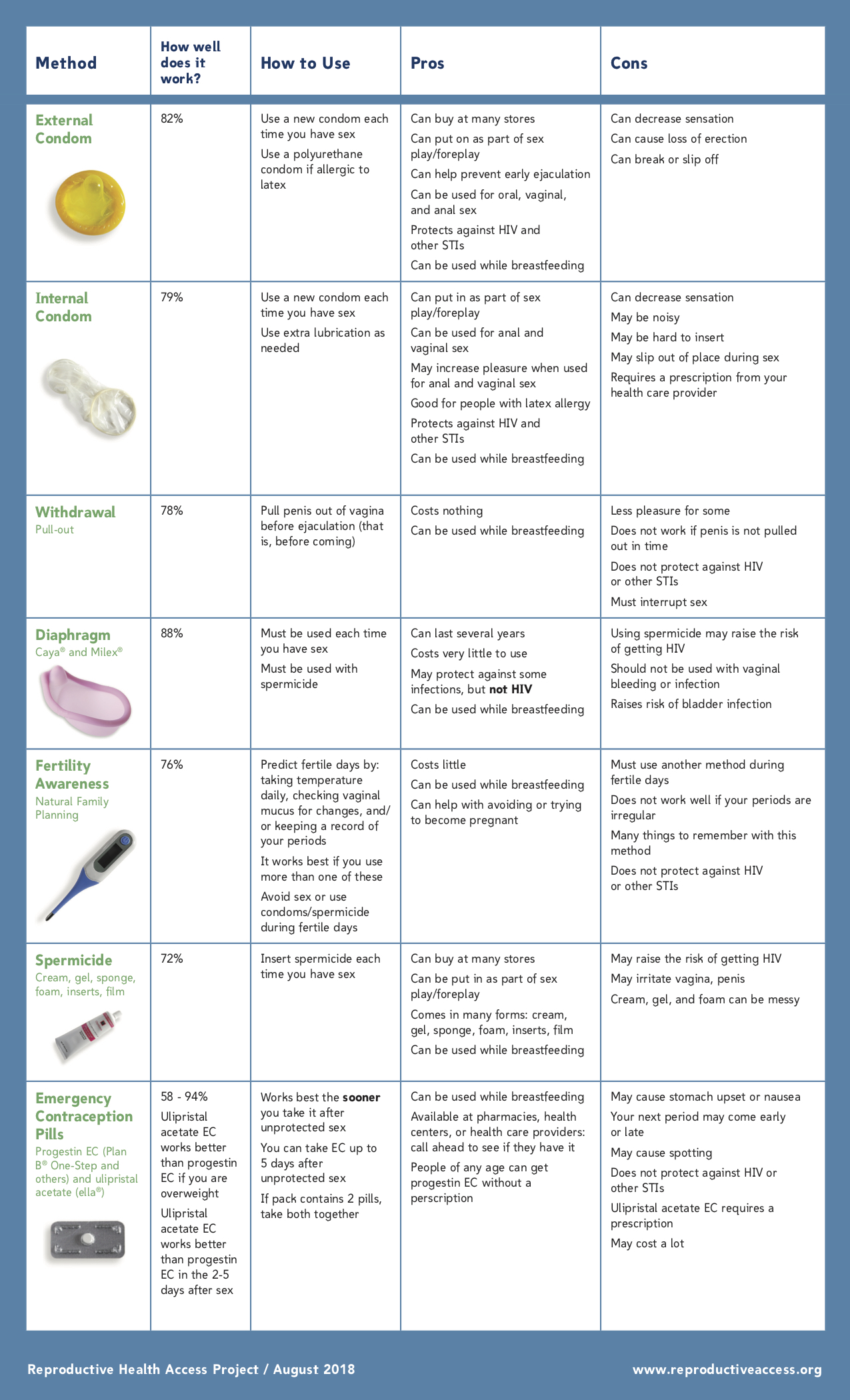
The following chart summarizes a variety of birth control options and their associated risks and benefits (The following chart summarizes a variety of birth control options and their associated risks and benefits (Reproductive Access, 2018):

Pregnancy
If you think you may be pregnant, the only way to really know is to get a pregnancy test. Many pregnancy tests will be accurate at the time your period is due. If a pregnancy test is done too early, it may not be accurate because the test cannot detect the change in hormones yet. The test may need to be repeated with an early morning urine sample or a few days later to be certain.
Home pregnancy tests can be bought at a drug store. You can also go to your health care provider or a clinic to get a pregnancy test.
If you are pregnant and not sure what to do, it can help to talk to someone about your options. What is best for you will depend on your life situation. Talk with your local health unit, youth clinic, or health care provider about supports to help you decide about the pregnancy.
Pregnancy and STIs
Pregnant people are usually tested for STIs including syphilis, chlamydia, gonorrhea and HIV as part of their prenatal care. STIs can be passed to the baby during pregnancy and delivery, and through breast/chest milk. Prevention and treatment is important in pregnancy because STIs can cause serious harm to a pregnant person and baby including premature labour, uterine infection, infant blindness, deafness and death. There are STI medications that are safe to take during pregnancy.
When a pregnant person has HIV, medication greatly lowers the chances of passing HIV to the baby.
(BC Centre for Disease Control, 2016)
Pregnancy and Substance Use
The harms associated with drug use during pregnancy are well-documented, but outright cessation is not a realistic option for many people. A harm reduction-oriented approach to pregnancy and substance use is needed.
Within a harm reduction framework, pregnancy is often described as an opportunity to support women and trans people in improving their health, including efforts to decrease or stop substance use, or increase safer use practices. Harm reduction approaches are a pragmatic response to substance use. They recognize that substance use is just one factor among many that shapes a healthy pregnancy and that reducing or stopping substance use at any time during pregnancy can have positive effects on a parent’s health and the health of the fetus (BCCEWH, 2015).
The following harm reduction strategies have strong evidence of effectiveness in the scientific literature and in practice as ways of supporting pregnant and new parents who use alcohol and drugs:
Education and outreach, including sharing information about safer drug use and distributing clean needles and other supplies
Low barrier access to services which emphasize physical and emotional safety, relationship-building, have short or no waitlists, and are provided in an accessible geographical location
Collaboration between health care and child welfare sectors that aims to support birth parents and their relatives and chosen families
Buprenorphine and methadone maintenance treatment
Provision of food vouchers, daily hot lunches, and prenatal vitamins
Testing for Sexually Transmitted Infections and other sexual health services
Addiction counselling, including help with quitting smoking
Assistance with transportation and child care to attend appointments
Access to integrated program models (e.g., on-site pregnancy-, parenting-, or child-related services offered with addiction services or coordinated referrals to other health and social services)
Research shows that harm reduction activities and approaches during pregnancy can:
Increase engagement and retention in prenatal services and addiction treatment
Increase referrals to other health and social services and increase engagement in services following birth
Reduce alcohol and drug use and improve nutrition
Reduce health care costs
Improve health outcomes for women, parents, and their babies, including fewer preterm births and babies born with low birth weight
Increase the number of babies discharged home with their parents following birth
Encourage breastfeeding, early attachment and improve early childhood development outcomes
(BCCEWH, 2015).
Homeless at Risk Prenatal Program
The Homeless at Risk Prenatal Program (HARP) in Toronto is an example of a local organization that uses a harm reduction approach to pregnancy and drug use.
HARP was implemented in 2007 after nearly ten years of lobbying for better healthcare for the city's pregnant homeless and transient women. Today, a dedicated team of nurses, dieticians and managers work closely with local hospitals, shelters and other organizations to ensure these parents have the safest pregnancy and the healthiest babies possible. Small victories are important to the HARP team and their community supporters. Victories can be as minor as getting a pregnant person to increase their protein intake with food coupons or as major as convincing them to give birth in a hospital. Success indicators give the team a good idea of how things are going for the client. For example: did the parent show up for their prenatal screening appointment this week? HARP also works very closely with Children's Aid to ensure the welfare of the parent and baby after birth.
(Canadian Public Health Association, n.d.)
References
BCCEWH. (2015). Harm reduction and pregnancy: Community-based approaches to prenatal substance use in western Canada. Retrieved from http://bccewh.bc.ca/wp-content/uploads/2015/02/HReduction-and-Preg-Booklet.2015_web.pdf
BC Centre for Disease Control. (2016). Smart Sex Resource. Retrieved from https://smartsexresource.com/
Canadian Public Health Association. (n.d.). Homeless at Risk Prenatal Program. Retrieved from https://www.cpha.ca/homeless-risk-prenatal-harp-program-toronto-ontario
Reproductive Access. (2018, August). Your Birth Control Choices. Retrieved from https://www.reproductiveaccess.org/wp-content/uploads/2014/06/contra_choices.pdf
